Blood cancers have paved the way for better therapies for many types of the disease
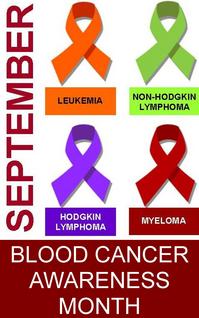
First a few facts. Collectively, the blood cancers — leukemia, lymphoma and myeloma — account for 9.5 percent of all cancers deaths, making them the second most common cause of cancer death, behind only lung cancer. Collectively, they also account for 9 percent of all new diagnoses in the U.S., making them the fourth most commonly occurring cancers behind lung, prostate and breast cancer.
More than a million adults in the U.S. are living with a blood cancer. The incidence of lymphoma has more than doubled since the 1970s. Scientists don't know why.
In children, leukemia and lymphoma account for nearly half of all childhood cancers. (And by the way, September is also Childhood Cancer Awareness Month.)
Despite having a long way to go, the mortality rate for many types of blood cancer has dropped significantly, thanks to strides that scientists have made in treating them. And the strides that have been made in the blood cancers have unlocked some of cancer's mysteries and paved the way for better treatments for many types of the disease.
It all began in the 1940s when researchers tested an agent related to mustard gas, the chemical warfare agent, in patients with non-Hodgkin lymphoma. Their improvement, though temporary, was remarkable, and it ushered in the era of treating patients with chemicals: chemotherapy.
In the 1950s, Boston pathologist Sidney Farber used another chemical compound to treat children with acute lymphoblastic leukemia. While remissions were brief, he proved that remissions were possible in a disease that had always been fatal. Soon, other chemotherapy drugs followed.
By the 1960s, scientists reasoned that a combination of drugs might be more successful, and they combined chemotherapy drugs for treatment of children with ALL. The disease went from being fatal to mostly curable.
This combination approach was then used to treat Hodgkin lymphoma, and again showed much greater success than a single drug. Soon, combinations of drugs were used to treat other types of cancer with better results than single agents.
But chemotherapy is highly toxic, and scientists dreamed of finding new treatments that would spare healthy cells while specifically targeting malignant ones. And they envisioned enlisting the body's own immune system to assist in getting rid of them.
But enlisting the body's own immune system would require engineering man-made antibodies which could specifically target and attach to malignant cells and then call the body's immune system in to destroy them. Man-made antibodies were first produced in 1975 by fusing normal B-lymphocytes from mice with human myeloma cells.
That discovery led to the first FDA-approved monoclonal (man-made) antibody treatment for cancer in 1997 — specifically, Rituxan, for treatment of non-Hodgkin lymphoma. This same drug has since been approved to treat rheumatoid arthritis. (Herceptin, well known for treatment of breast cancer, is another monoclonal antibody).
At the University of Michigan, Dr. Mark Kaminski took monoclonal antibody therapy a step further. He combined monoclonal antibodies with radioactive isotopes (molecules) which resulted in a treatment known as radioimmunotherapy, which not only calls the body's own immune system into action, but also — for a dual action and extra lethal effect — delivers radiation directly to the tumor.
Dr. Kaminski's first clinical trial opened in April 1990. His drug, Bexxar, and another RIT drug, Zevalin, were approved by the FDA for treatment of some forms of non-Hodgkin lymphoma in 2002 and 2003.
But calling in our immune systems to fight cancer wasn't the only way scientists were thinking about stopping the disease. Since uncontrolled growth is the hallmark of cancer cells, they wondered if something in our genes might cause uncontrolled growth.
The first genetic abnormality to be identified in any cancer was identified in chronic myelogenous leukemia. In 1960, scientists discovered that parts of two chromosomes switch places during the process of cell division, resulting in an abnormal gene which causes uncontrolled growth.
Developing a treatment to interrupt the malicious behavior of abnormal genes would take years of dedicated research and better technology. Finally, in 2001, Gleevec was the first drug approved by the FDA to specifically target and inhibit the activity of proteins produced by the abnormal genes in CML.
More importantly for patients, Gleevec turned CML from a fatal disease into one that can almost always be managed as a chronic illness. And it proved that targeting genetic abnormalities could stop cancer's deadly march.
By 2011, Gleevec had been approved to treat not only CML but also a handful of other types of rare cancers.
Scientists dug deeper into the biology of cancer cells and came up with other targeted therapies that either inhibit, inactivate, block or otherwise destroy them. Today, the National Cancer Institute lists 42 targeted therapies approved to treat a variety of cancers. Many more are in clinical trials.
Indeed, discoveries in blood cancers have helped to inform scientists about the genetic abnormalities of cancer and helped lead them to develop targeted therapies against them, but blood cancers aren't just leading the way in targeted therapies. It was a blood cancer that gave scientists a glimpse of why cancer might recur.
In the mid-1990s, a Toronto biologist identified a small population of cells within acute myelogenous leukemia. This small population of cells, called cancer stem cells, had the ability to sustain cancer after therapy and cause recurrence.
Few scientists believed that cancer stem cells existed, much less that they could be found in solid tumors, but Dr. Max Wicha, director of the University of Michigan's Cancer Center, did. In 2003, he and his team identified cancer stem cells in breast cancer. Soon, cancer stem cells were identified in other solid cancers and the hunt to find drugs that will destroy them — and prevent metastasis — is on.
There's a lesson in all this. Scientists learned it years ago: What's learned about one cancer might be applied to another. That's why they're working collaboratively and across specialty lines to push progress forward faster.
It's natural for us lay folks to pay attention to the cancer that's impacted us, but the fact is, we're all after the same thing: a cure. Since none of us knows where the next breakthrough will come from or how it will be applied to the cancer we care about, I'm cheering every stride made in every cancer and the scientists who are working hard to make them.
Betsy de Parry is the author of Adventures In Cancer Land. Find her on Facebook or email her.


Comments
iraj ahmed
Sat, Sep 15, 2012 : 6:43 p.m.
blood cancer is one of the common disease in our country ( bangladesh) .maximum people are under poverty line.that's why they can't take proper treatment.my question is it possible to reduce treatment cost? "MedsempireImran"
iraj ahmed
Sat, Sep 15, 2012 : 6:41 p.m.
blood cancer is one of the common disease in our country ( bangladesh) .maximum people are under poverty line.that's why they can't take proper treatment.my question is it possible to reduce treatment cost? http://www.medsempire.com
LA
Mon, Sep 3, 2012 : 2:29 p.m.
Great article, thank you!
Technojunkie
Sun, Sep 2, 2012 : 2:32 p.m.
I wonder how much blood cancer is caused by mercury poisoning from half-mercury "silver" dental fillings. Improper removal of amalgam fillings gives the body a big blast of mercury. It's easy to test for, a chemist named Andrew Cutler figured out the rules for hair test interpretation, but we all know that multiple grams of mercury are perfectly safe when put into a person's mouth because the ADA said so.